By Ted Alcorn/ New Mexico In Depth
Alcohol is killing New Mexicans at a higher rate than anywhere else in the country — yet the state has largely neglected the growing crisis. In this seven-part series from News Port partner New Mexico In Depth, journalist Ted Alcorn investigates the state’s blind spots and shines a light on solutions.
Stereotypes about alcohol and Native people are hiding a crisis that’s bigger than any single group.
The forecasted low in Gallup is 17 degrees, cold even for February, but the man’s jacket is unzipped when the headlights find him slumped against a darkened storefront, a Broncos cap pulled over his eyes. “I’m going to get you some place warm,” Public Safety Officer Gabriel Lee Jr. says as he helps the man into the back of the police van.
In a downtown hospital emergency room, where most clinicians attend to urgent injuries or illness rather than their underlying causes, licensed professional clinical counselor Sheryl Livingston asks a Navajo patient what she enjoys most about alcohol. The patient laughs in surprise, then begins to open up.
Outside a new drug and alcohol treatment facility in a sandy lot, a circle of men sit sweating beneath the domed canvas of a hogan, a pile of volcanic rocks fresh from the fire glowing faintly between them, their folded knees close enough to touch. Medicine man Robinson Tom asks for a prayer and a dozen voices mingle Diné and Spanish and English in the stifling heat.
Night and day, people across Gallup struggle with alcohol, in a community that for decades has borne some of its most devastating impacts. In surrounding McKinley County, the rate of alcohol-induced deaths is more than three times the state’s and 10 times the nation’s.
Because Native Americans make up 80% of the county’s residents — and bars and liquor stores in Gallup draw customers from the neighboring Navajo Nation and Zuni Pueblo, where alcohol possession and consumption are forbidden — the place is emblematic of a popular myth: that New Mexico’s alcohol crisis primarily affects Native people.
It’s false. Even if the mortality rate for Native people was in line with Anglos and Hispanic residents, the state would still have a crisis of alcohol deaths on its hands.
A New Mexico In Depth analysis of mortality data shows that Anglos and Hispanics in New Mexico also die at rates far surpassing their counterparts elsewhere, and together account for 80% of the state’s alcohol-induced deaths. Even excluding Native deaths, over the last five years of data New Mexico still had the highest rate of alcohol-induced deaths of any state.
“It’s not just Natives who have struggled with this issue,” said Michelle Brandser, a member of the Navajo Nation and the Health Services Administrator for the tribe’s Division of Behavior and Mental Health Services.
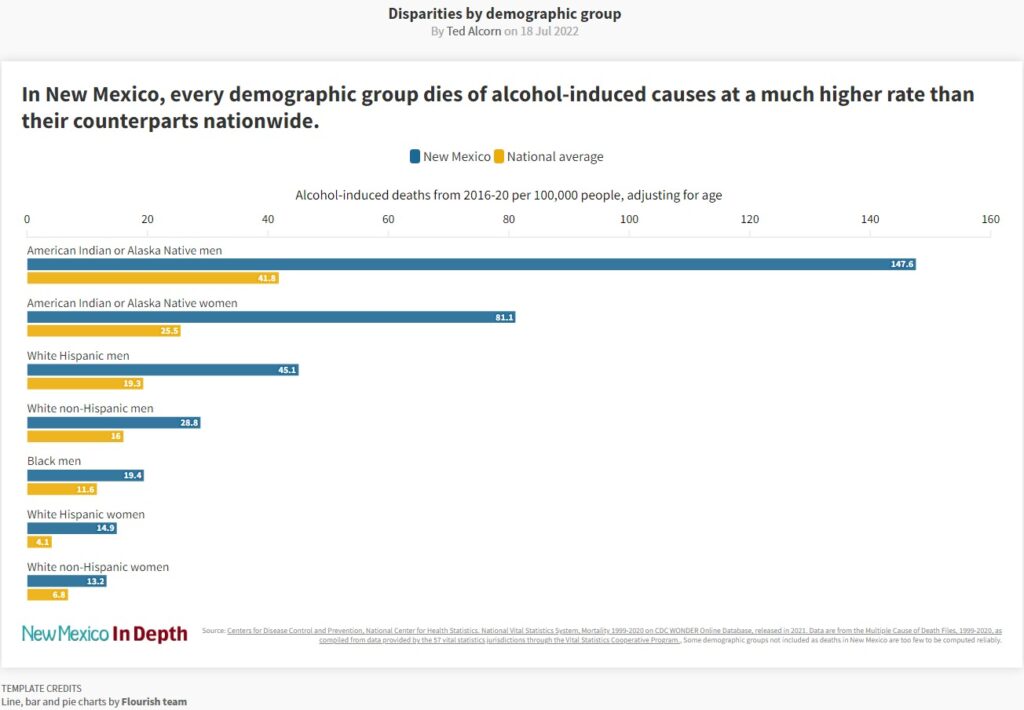
The disparities, nonetheless, are grave. In the early 1990s, David Jernigan, now a professor at the Boston University School of Public Health, did research in Gallup including a night spent in the town’s infamous drunk tank, a cement room where police deposited inebriated people they had picked off the street. “It was observable genocide,” he recalled. The drunk tank is gone now but the community’s problems have worsened. Among Native men of working age in McKinley County, the alcohol-induced death rate is 385 per 100,000 — higher than the gun homicide rate of Black teenage boys in Chicago.
The enduring question is what to do about it, and who is to do it. Individual drinkers have some responsibility but the focus on alcohol misuse by Native Americans distracts from the larger context: McKinley County’s elevated rate of alcohol-related death is a product of unequal treatment of Indigenous communities and the state’s lax policies governing alcohol sales.
That, Brandser said, should be a call to action for all New Mexicans. “It’s got to be a shared responsibility.”
The deflection of blame
Falsehoods about Native people and alcohol are commonly held and age-old, said Philip May, a professor at the University of North Carolina at Chapel Hill who has devoted his career to studying alcohol and is married to a member of the Laguna Pueblo Tribe. “For as long as I’ve been alive—74 years—there’s always been a perception that American Indians drink to excess; that they have a biological susceptibility to intoxication,” he said.
The belief is widely held among Native people themselves. And practicing clinicians in Gallup and Albuquerque, who regularly treat alcohol disorders, refer to “something genetic” or a “predisposition” to explain different outcomes they perceive among their Native patients.
These views are wrong, according to Kamilla Venner, an associate professor of psychology at the University of New Mexico (UNM), who is of the Ahtna Athabascan people in Alaska. “There are no biological differences in American Indian / Alaskan Natives that are contributing to these health inequities,” she wrote in an email.
Although studies show that heredity accounts for about half a person’s propensity for addiction, there has never been evidence that Native Americans’ genes expose the group as a whole to greater risk. Surveys routinely find that the share of Native Americans in New Mexico who consume alcohol is lower — not higher — than that of other racial and ethnic groups.
The myth matters because it strips Native people of their agency, said Spero Manson, a professor of public health and psychiatry at the University of Colorado who is Pembina Chippewa. “[It] fuels an often-observed assumption in tribal communities that alcohol and addiction is our destiny,” he said.
Attributing alcohol’s elevated harms to genetics also ignores the vastly unequal historical experience of Native people, from the conquest of New Mexico that stripped tribes of their land, to the boarding school system that ripped apart families, to federal control today that barely fulfills their basic needs.
No other population in New Mexico experiences similar levels of poverty, nor has been subject to a comparable attempt to destroy its cultural foundations.
Counselor Sheryl Livingston said her people, the Navajo, continue to suffer from these historical traumas. Violence meted out on bygone generations — “having your family murdered in front of you, raped, your crops destroyed, your house burned down” — still reverberates.
The consequences of that unequal treatment are evident across a range of health disparities experienced by Native people, who are 1.8 times as likely as other Americans to die of influenza and pneumonia, 2.5 times as likely to die in accidents, and 3.2 times as likely to die of diabetes.
But even this explanation — that alcohol misuse is a regrettable but understandable response to past oppression — can deflect attention from present-day causes of disparities. Kara Roanhorse, a Navajo and member of The Red Nation, a coalition that seeks the liberation of indigenous peoples and the repatriation of their land, said it frames the issue too narrowly, as, “The Native people are the problem, and it’s the Native problem that needs solving.” In fact, she said, bigger systems of colonialism and capitalism are the cause.
In a recent book chronicling the life of Navajo student activist Larry Casuse, who died trying to close down an infamous bar outside of Gallup, UNM professor David Correia pointed to industries long known for preying on the community: payday lenders that charge usurious rates, unscrupulous art dealers who exploit Native craftspeople, and bars and liquor stores that profit by selling an addictive substance to a population prohibited from drinking in their own homes.
By law, a town of Gallup’s population is limited to 11 businesses licensed to sell alcohol. There are currently 30 operating, according to data obtained from the state Regulation and Licensing Department (down from 61 in 1988).
Poor health outcomes in the town are “not an aberration or product of past colonial conquest,” Correia wrote; the very poverty and inequality they reflect are what makes the economy of Gallup possible.
A history of leadership
For both good and ill, New Mexico’s leaders have spotlighted alcohol misuse in Gallup, singling out one community while ignoring it everywhere else.
In 1986, Ed Muñoz was elected mayor on his promise to address Gallup’s problem. He had a combative style, at one point proposing billboards that depicted a road paved with skulls and warned visitors they were entering the “drunken driving capital of the world.” Critics nearly succeeded in recalling him from office.
He managed to attract the attention of The Albuquerque Tribune, which in 1988 published a six-part series about alcohol in Gallup entitled “The Killing Season.” The journalists identified local businesses profiting from addiction, including a company that imported cheap fortified wine by the tractor trailer and sold it by the pint under the label Garden Deluxe. They also noted that Gallup’s alcohol industry reported more taxable earnings in 1987 than all its finance, insurance, and real estate businesses combined.
But the series, brimming with stigmatizing photos of inebriated Native people, left an impression that Gallup was deviant and in denial. Although a newspaper editorial acknowledged that “every community, including Albuquerque, has a drinking problem,” the series was preoccupied with the town of 19,000 people.
Then in Gallup on January 14, 1989, an intoxicated driver collided with a family on their way to church, killing three people including an infant, Katherine “Jovita” Vega.
Muñoz and local organizers announced they would march 200 miles from Gallup to Santa Fe. The next month in what they dubbed the “Journey for Jovita,” hundreds set off on foot, including children and elders, teachers and executives, and people struggling with alcohol dependence. The marchers braved the elements and traffic on the interstate for 10 straight days. By the time they arrived at the capital, the crowd had swelled to 2,000, and papers around the country were covering their trek.
“It definitely got the attention of all the legislators,” said Gallup’s present-day Mayor Louis Bonaguidi, who had just been elected to city council and drove to Santa Fe for the final leg. “They basically shut down all the committee meetings and everything, and had a joint session.”
The lawmakers allowed McKinley County to move forward with a local ballot measure that would ultimately close its drive-up liquor windows and impose a 5% tax on alcohol sales in the county. Some of the revenues paid for a more humane detoxification center where inebriated people can safely sober up and enter treatment, replacing the notorious drunk tank.
Later that year, Gallup’s city council passed an ordinance lowering the legal blood alcohol limit from .10 to .08. Inspired by the citizens’ commitment, the Robert Wood Johnson Foundation gave a local organization the first of what would be over $5 million in grants to support their efforts to reduce substance use.
The state would ultimately follow Gallup’s lead, closing drive-up windows and lowering the legal blood alcohol limit statewide.
But in other ways, lawmakers have continued to treat McKinley County as an exception instead of learning from its practices. In 2021, when the Legislature made rare changes to alcohol laws, Sen. George Muñoz, son of the former Gallup mayor and chair of the powerful Senate Finance committee, successfully amended the legislation to bar gas stations in McKinley County from selling hard liquor. (At least three promptly shuttered their gas pumps instead.)

During a legislative hearing, Sen. Antionette Sedillo Lopez, D-Albuquerque, observed: “It feels like it’s singling out one community when there are so many other communities that are similarly situated.” The alcohol-induced death rates of Native people in Rio Arriba and Socorro counties exceed that of McKinley, according to CDC data.
But fundamental inequalities continue to afflict the area: 32% of McKinley County residents live below the poverty line compared to 17% statewide, and the elevated unemployment rate, lack of transportation, and layers of historical trauma contribute to further alcoholism.
All of which helps explain why, in spite of local efforts to enact protective policies, McKinley County’s alcohol-related death rate has worsened, and the gap between it and the state has widened.
According to Sindy Sacoman, an evaluator who works with the county on behavioral health issues, “The issue is so big that one program or one community can’t address all of it.”
The everyday struggle
“Alcoholism didn’t quite destroy my immediate family, but I did see a lot of destruction,” Raechelle Morgan said. “It’s a common language for us out here.”
Born on the Navajo reservation in nearby Crown Point, Raechelle is the youngest of four. Her dad worked as an artisan and her mom was a teacher, and the family valued education. “It wasn’t a luxury. It wasn’t a choice,” she said. “It was like: you are going to school for your own survival.”
When Raechelle was in elementary school the family moved to Albuquerque so her mom could finish a master’s degree, and the kids struggled to fit in. Her brother Myron, the closest to her in age, was often bullied in his predominantly Anglo school and grew up fighting.
Still, the siblings excelled academically — Myron graduated early with honors and went straight into a college program in Grants.
They also drank regularly at school. Looking back, Raechelle said she was an alcoholic by the time she reached high school, as were many of her peers. “I don’t remember much of my 16th year, that’s how much I drank.” Her parents were concerned but didn’t seem to know how to address it. “The times went a lot faster than we did.”
On the night of a reception for Raechelle’s high school graduation, she and her brother and cousins went out to celebrate. They had been drinking, and when they stopped at a store, Myron ran into some guys he knew and they argued. In the fight that followed, he was knifed in the groin, and the ambulance took a long time to arrive. He bled to death on the way to the hospital, at the age of 19.


Raechelle’s father retreated to Myron’s truck and slept there for days after his son’s death. But it also gave the family a sense of urgency about confronting substance use in their midst. “We finally saw in our family what alcohol could do,” Raechelle recalled.
Raechelle is now part of a younger generation in Gallup that is doing all it can to comprehensively treat alcohol disorders.
After her brother died, her mom helped her complete college applications through a haze of grief. One was for Western New Mexico University, which had a burgeoning chemical dependency counseling program. Already interested in the field, the death of her brother gave Raechelle the terrible knowledge of “how it felt to be on the other side — the vulnerable population, the one that needed help.”
Today, years after completing the program, she is back in Gallup helping treat drug and alcohol use as one of the primary clinicians at the Four Corners Detoxification and Treatment Center, which opened last year in a former juvenile detention facility east of town.
Another leading local figure is Dr. Jennie Wei, a Harvard-trained internal medicine physician working at Gallup Indian Medical Center (GIMC). The hospital is part of the Indian Health Service, which has about a third the resources for each patient that other Americans enjoy but still attracts committed and rigorous clinicians.
There, Wei is pushing more assertive screening and treatment of alcohol disorders. During her residency at the University of California San Francisco Medical Center, she established protocols to ensure alcohol dependent patients were screened and offered the FDA-approved medication naltrexone to help fight their cravings. Upon arriving in Gallup in 2012 she replicated the program. The number of patients at GIMC who are receiving naltrexone has risen 20-fold in the years since, from 25 in 2012 to 525 in 2021.
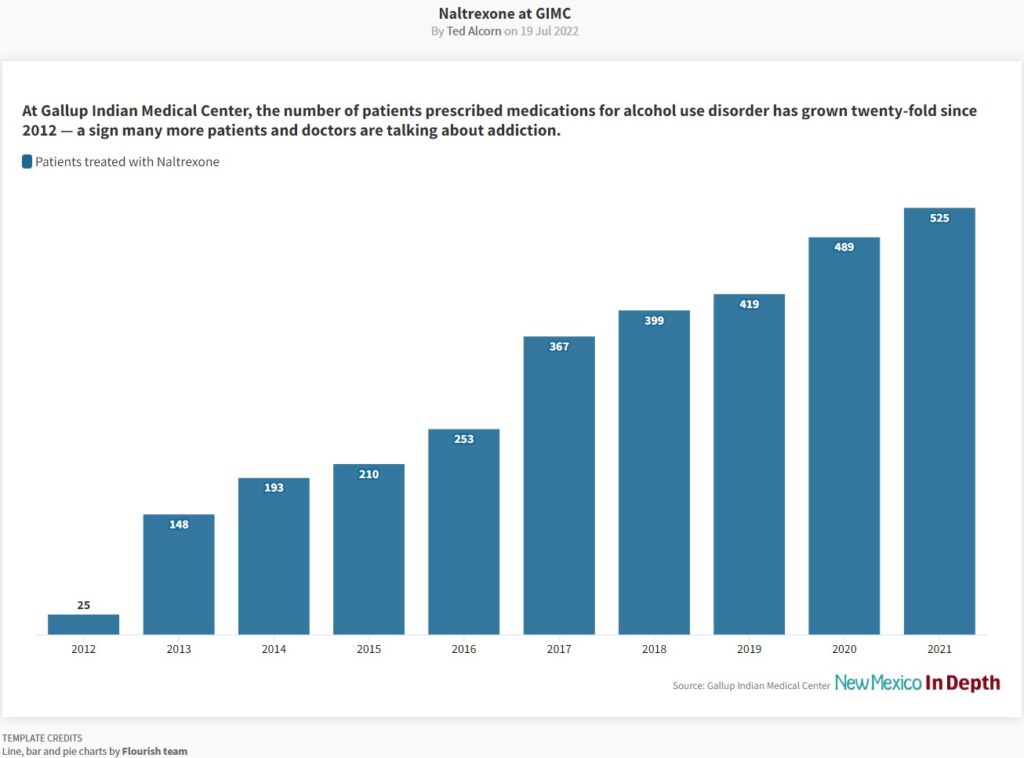
More important than the medication, Wei said, is creating space for clinicians and patients to talk openly about alcohol. “I’m most excited that 525 people had a conversation with their provider about their substance abuse,” she said.
Wei also helped create a full-time role screening for alcohol use in the hospital’s emergency room, and in 2014 she launched the Gallup-McKinley County Task Force on Alcohol, a bi-monthly meeting point for public agencies, tribal authorities, and treatment providers to coordinate their work.

Meanwhile, Native patients and clinicians are trying to reclaim their history and spirituality, including in the therapies offered for alcohol disorders.
Venner, the UNM professor, said that people who learn their culture’s traditions and assimilate its values—whether by participating in ancestral practices, speaking a native tongue or partaking in religious ceremonies—are better able to deal with alcohol disorders. For some patients, substance use treatments that incorporate those elements are more meaningful and helpful. “What I hear from more traditional people is that, in order to be well, they have to know where they come from, and who they are, and what their cultural identity is,” she said.
The sweat lodge that Four Corners holds on Saturdays is a prime example. The ceremony has not been rigorously evaluated as a substance use treatment, Raechelle observed, but patients look forward to it more than any other session. Its sweltering intimacy, filled with songs and prayers, offers “a stripping down of cognitive defenses,” she said. “You get to the emotional part of your senses, and sometimes it’s a safe place to be vulnerable.”
As the men finish their sweat, Robinson Tom, the medicine man, speaks to them about the limits of the ceremony’s powers. “The enemy is waiting for you out there, when you go back — people that used to drink with you.” He cautions: “It’s gonna be up to you.”
Speaking to the other men, a patient describes his arrival at the facility one month earlier, addicted and suicidal. “I got the answers I needed,” he reflects. “I was always taught not to cry, and now I love to cry. I know how important it is. And I can be okay with my emotions today.”
The men’s voices rise and fall. Finally spent, with calls for the door to open, they file out to drink water, their sweat drying quickly in the bright, dry, still, late-morning light.
Ted Alcorn is a writer raised in New Mexico whose work has appeared in The New York Times, The Atlantic, and The Washington Post Magazine, among other publications. For New Mexico In Depth he’s investigated how the state’s prisons have ignored an epidemic of hepatitis C, how Albuquerque stood up its branch of non-police emergency response, and how non-profit hospitals shortchange community health. Follow him at @tedalcorn.
This story was originally published by New Mexico In Depth