Providers don’t prescribe drugs like buprenorphine, the gold standard for treatment. Why?
By Vanessa G. Sánchez/ Searchlight New Mexico
ALBUQUERQUE — Jennifer Daniels had tried to quit heroin many times, but the cravings and withdrawals — the stomach cramps, chills and fevers — always won over.
In 2013, when she learned she was pregnant with her third child, she was terrified for the baby’s well-being. But then she found her way to a prenatal program in Albuquerque, where doctors prescribed a medication that’s long been considered the gold standard for helping pregnant women with substance use disorder: buprenorphine.
Three months later, her baby was born — a healthy girl, now 9 years old. As for Daniels, she has been in recovery for nine years, thanks to psychotherapy and Suboxone, a combination of buprenorphine and naloxone.
“I don’t know if I could have done without it,” said Daniels, 36, who works with formerly incarcerated youth as a program coordinator at the UNM ADOBE Program in Albuquerque. “This medication allowed me to be there with my family and allowed me to then find a job and work that job.”
But in 2014, her appeal for help came with a punishing consequence. Roughly a month after giving birth, Daniels lost custody of her infant and two older daughters.
“It felt like my heart was ripped out of my chest,” she said. A year went by before she got her children back.
Daniels’ story reflects New Mexico’s changing policies regarding women with substance use disorder and the state’s flawed attempts to render help. At the time of her third pregnancy, it was up to individual hospitals whether or not to report a case of neonatal drug exposure to state authorities, according to the Children, Youth and Families Department (CYFD).
That changed in 2019, when New Mexico enacted legislation that shifted its approach to align with federal standards. The state embraced the Comprehensive Addiction and Recovery Act, a nationally recognized effort that was intended to keep families intact and make it easier for pregnant women and their infants to get medical treatment and wraparound services. Today, a positive screening for drugs is no longer — on its own — grounds for referral to CYFD.
But without the right treatment, the policy falls short of providing help.
“If you aren’t going to take care of the mother so that she can be successful, then what gives us the authority to take their child away before they even have a chance?” said pediatrician Andrew Hsi, who helped spearhead the 2019 legislation when he was the director of the UNM Institute for Resilience, Health and Justice. Though now retired, Hsi is still revered for his work in the field.
Good on paper, not in practice
New Mexico has come a long way — at least on paper.
In practice, however, few pregnant women have managed to access treatment for opioid and other substance use disorders. Between 2016 and 2019, an estimated 17,000 pregnant women in New Mexico used a drug of some kind, whether that meant opioids, methamphetamine, cocaine or other substances, according to the most recent available data from the Department of Health. Only 3 percent of those women received treatment for their substance use.
Searchlight New Mexico contacted all 28 hospitals in the state that provide maternal health services, asking each if they offer medication treatment for opioid use during and after pregnancy. Three did not respond and one declined to comment.
Of the remaining 24 hospitals, 14 reported that they offer the recommended medications for opioid use during and after pregnancy. Two said they don’t prescribe to new patients but will write prescriptions for pregnant women already on the medications. The other eight — mainly rural hospitals — reported that they do not offer these medications at all.
Overdose deaths soar
The opioid crisis has hit New Mexico hard. More than 130,000 residents — a population about the size of Las Cruces — have a substance use disorder for which they receive no treatment, according to a 2021 Legislative Finance Committee report.
Overdose deaths in the state nearly doubled in the first two years of the pandemic, mirroring a national increase that in 2021 reached 100,000 U.S. deaths a year. The majority were attributed to fentanyl, a synthetic opioid up to 50 times stronger than heroin. The spike has taken a toll on people of color and a subset of the population often overlooked: pregnant women.
In New Mexico, substance use disorder — the recurrent use of alcohol or drugs that causes significant impairment — is one of the leading contributors to maternal deaths, both during and within a year after pregnancy. That trend is also on the rise across the nation: A 2022 Columbia University study found an 81 percent increase in drug overdose deaths among pregnant women between 2017 and 2020, including a large increase in deaths involving fentanyl and drugs like methamphetamine.
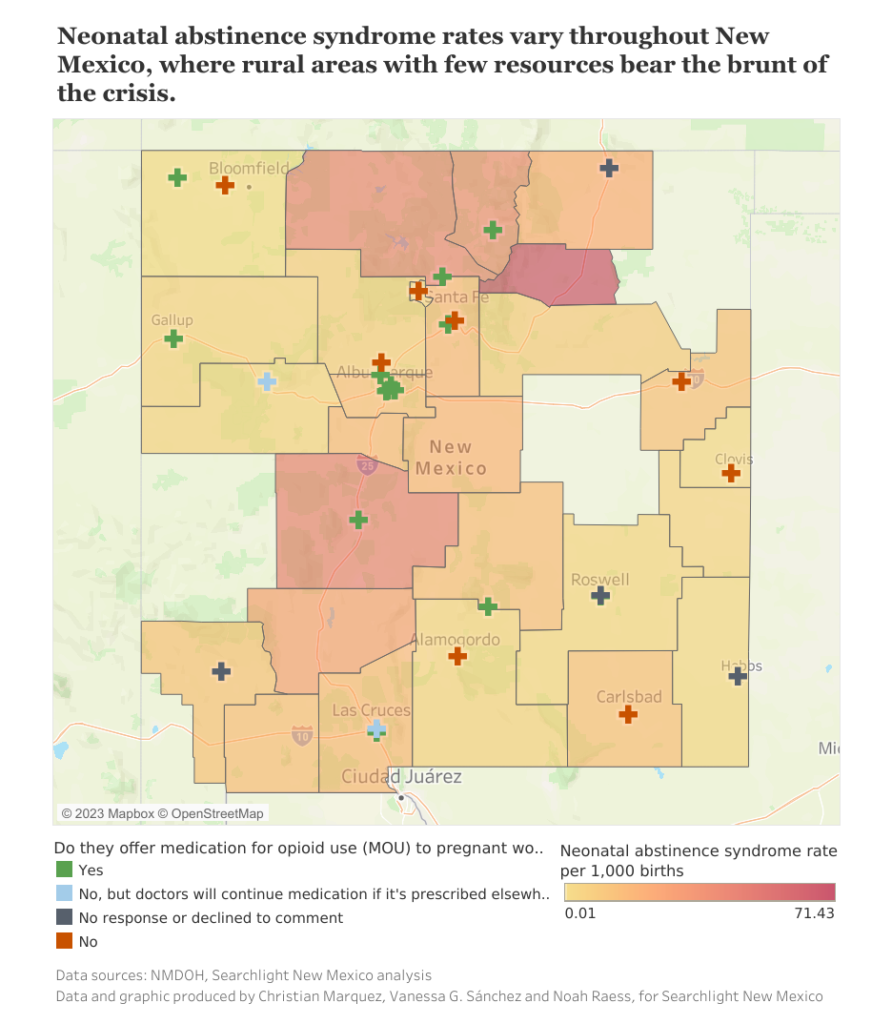
Substance use has taken a similar toll on infants. The rate of hospitalizations for neonatal abstinence syndrome (NAS) — a group of conditions associated with withdrawal symptoms when an infant has been exposed to a substance in the womb — tripled between 2010 and 2020 in New Mexico, rising from 4.3 to 13.6 per 1,000 newborn hospitalizations, an analysis of health data shows.

In 2020, some 260 infants were hospitalized with NAS, more than double the number hospitalized a decade earlier. The number of NAS cases in 2021 ranged from zero in places like De Baca and Guadalupe counties to four in McKinley, 18 in Rio Arriba, 21 in Santa Fe and 45 in Dona Ana counties. The highest number of cases — 98 — was in Bernalillo County.
While NAS rates were higher in New Mexico’s cities, small and rural towns saw the largest rate increases, federal statistics showed, with most cases occurring among newborns on Medicaid, whose mothers often lack access to quality care.
Experts said multiple other factors help explain the increases. Among them: Screening for substance use is now standard, so hospitals are identifying and diagnosing NAS more frequently. In addition, while substance use disorder grew over the decade — and soared at the start of the pandemic — access to treatment has remained limited, especially in small, rural communities.
But there is another, overarching problem, specific to New Mexico. The state has failed to provide the necessary resources and funding to comprehensively help mothers and infants, according to many advocates and medical experts. Under the 2019 legislation, for example, state agencies and providers were supposed to implement a “plan of care” for women with substance use disorder, to ensure they received postpartum health care, housing assistance and treatment. But there’s been little follow-through.
“When we presented this legislation, we made it clear that after the plan of care was developed there would need to be a way of implementing the program,” said Hsi. “The legislature and [cabinet] secretaries have not stepped up to make that happen.”
Life-saving medications go unused
Buprenorphine and other related medications work by binding to the receptors in the brain that crave opioids, preventing withdrawal symptoms in the mother and averting long-lasting complications for the baby. When accompanied by therapy and prenatal care, they help mothers sustain addiction recovery, support a full-term pregnancy and achieve better outcomes after birth, according to the American College of Obstetricians and Gynecologists and the Centers for Disease Control and Prevention.
These same medications have also been shown to benefit infants, leading to shorter hospitalizations and less need for morphine or methadone.
“When you think about how good these drugs are at preventing something bad, it works incredibly well,” said James Besante, an addiction medicine specialist and chief medical officer at the Santa Fe Recovery Center. “The sad reality is that most patients, including pregnant women, do not have access to this life-saving medication.”

Pregnant women lack access to prenatal care throughout the state. In the last decade, six hospitals closed their maternity units, while at least three clinics shuttered or severely reduced operations, due to financial stress, staff shortages and other causes. These closures have resulted in “maternity care deserts” — entire counties in which medical access has disappeared or been severely curtailed.
“Even if we could find someone to prescribe them buprenorphine or if there was a methadone clinic there, they might not have a place to deliver,” said Francheska Gurule, a family practitioner at the UNM Milagro Program, which provides maternal care, infant care and addiction treatment in the same setting. “If they do have a place to deliver, they’re not really equipped to manage their pain or take care of their babies who are experiencing withdrawal.”
Huge needs, zero treatment
Three rural counties illustrate the problem. Valencia and Torrance, south of Albuquerque, are maternal health deserts, as is Luna County, near the Mexico border: All three have limited access to medication for opioid addiction. Of all New Mexico counties, they have experienced some of the highest rate increases of NAS in the past decade, according to a Searchlight analysis.
In Otero County, at the state’s southern edge, one of the only clinics to prescribe medications closed its doors four years ago. Today, the county’s only hospital — Gerald Champion Regional Medical Center — does not prescribe the medications but instead refers pregnant patients to outpatient clinics, mainly in Albuquerque, a hospital spokesperson said. Albuquerque is a three-hour drive away.
“There is just not enough treatment in general, but then when you add the layer of being pregnant, it becomes even worse,” said LuzHilda Campos, deputy director at Bold Futures, a statewide nonprofit that advocates for reproductive rights. “There are towns that have been ghosted completely, and those are the towns where we see the highest use and the highest need for these resources.”

‘Tremendous burden of shame’
A prevailing stigma is at the heart of the resistance to treatment, according to providers. Some doctors are simply uncomfortable treating addiction and prescribing medication, even though it’s now regarded as the gold standard. And pregnant women, fearing judgment, are less likely to seek treatment promptly — or at all.
“The odds are really stacked against them,” Besante said. “They’re marginalized by society and stigmatized for their substance use. There’s a tremendous burden of shame thrust on these women.”
Last December, a change in federal law eliminated the need for doctors to obtain a special waiver to prescribe buprenorphine. The waiver elimination makes it possible for doctors throughout the country to prescribe buprenorphine to an unlimited number of patients. Yet, the number of buprenorphine prescribers in New Mexico has not significantly increased.
In addition, the vast majority of doctors in the state still prescribe it to fewer than 10 people, according to monthly opioid prescriber reports between December 2022 and March 2023 reviewed by Searchlight.
In her workshops with rural hospitals, Gurule from the Milagro Program found that some providers were still unaware that the waiver had been lifted.

Few bridges to treatment
In 2020, the state launched New Mexico Bridge, a program to encourage medical treatment for opioid addiction in emergency departments in rural hospitals.
Six hospitals so far have joined the program and agreed to expand their medication treatment services, according to Margaret Greenwood-Ericksen, the program’s engagement and dissemination director, who reaches out to hospitals and helps them get started. A few have resisted.
“Some of the hospitals feel like they still can’t overcome rural workforce barriers, and then of course the other issue is just stigma,” Greenwood-Ericksen said. “We have had some clinicians at some hospitals tell us they don’t think that these medications like buprenorphine should be prescribed in the emergency department.
“We have to do a lot of corrections and education around stigma.”
Noah Raess and Christian Marquez contributed to this story.
Vanessa G. Sánchez Born and raised in Ecuador, Sánchez has written in-depth stories about issues affecting underrepresented communities, including migrant workers and asylum seekers in the U.S. She contributed to the award-winning investigations “Essential and Exposed” and “Printing Hate.” As an intern and Bradlee Fellow at The Washington Post, she covered education, local government and politics in the Baltimore-Washington region. She joins Searchlight as a yearlong Roy W. Howard fellow to cover health policies affecting children and families in New Mexico. Sánchez holds a master’s degree in journalism from the University of Maryland.
Searchlight New Mexico is a nonpartisan, nonprofit news organization dedicated to investigative reporting in New Mexico.
